Designing Mental Health Education Programs: Lessons from Kaiser Permanente Arvada
Mental health education programs at facilities like the Kaiser Permanente mental health facility in…….
In the ever-evolving landscape of healthcare, the focus on mental well-being has become a paramount priority, driving significant advancements in specialized treatment facilities. Among these, the Kaiser Permanente mental health facility in Arvada, Colorado, stands as a beacon of hope and innovation. This comprehensive article delves into the intricacies of this renowned institution, exploring its history, impact, and future trajectory. By examining its various facets, we aim to provide valuable insights for healthcare professionals, policymakers, and individuals seeking understanding in this critical domain.
The Kaiser Permanente mental health facility in Arvada is a state-of-the-art medical center dedicated exclusively to the diagnosis, treatment, and prevention of mental health disorders. It forms part of the larger Kaiser Permanente healthcare network, known for its comprehensive, patient-centered approach. The facility offers a wide array of services, including outpatient therapy, psychiatric medication management, crisis intervention, and specialized programs tailored to specific conditions such as depression, anxiety, bipolar disorder, and schizophrenia.
Arvada’s mental health facility traces its roots back to the early 1970s when Kaiser Permanente, a leading healthcare provider in the United States, recognized the growing need for specialized mental health services. The establishment of this facility marked a significant step towards integrating mental health care into the primary healthcare system. Over the years, it has evolved to meet the changing needs of its community, incorporating new treatment modalities and technologies.
This facility’s significance lies in its ability to provide accessible, high-quality mental healthcare to a diverse population. By offering comprehensive services under one roof, it reduces barriers to care, ensuring individuals receive coordinated and continuous support throughout their recovery journey.
Within the broader landscape of mental health care, Kaiser Permanente Arvada stands as an exemplary model of integrated healthcare delivery. It embodies the principles of patient-centered care, emphasizing holistic treatment approaches that consider physical and mental well-being. This facility’s success contributes to a growing movement towards destigmatizing mental illness and promoting equitable access to care.
The Kaiser Permanente model has garnered international recognition for its innovative approach to mental health care. Its focus on community-based, accessible healthcare has inspired similar initiatives worldwide. Many countries are adopting elements of this model to strengthen their mental health systems, particularly in addressing the gap between primary care and specialized services.
Several key trends are shaping the trajectory of Kaiser Permanente-inspired facilities globally:
Integrated Care Models: There is a growing emphasis on integrating mental health services into primary care settings, mirroring the Kaiser model. This collaborative approach ensures early intervention and continuous support for patients with mental health conditions.
Telehealth and Digital Health: The adoption of telehealth technologies enables remote access to mental health services, particularly beneficial in rural or underserved areas. Mobile apps and digital platforms are also being utilized for self-monitoring and peer support, enhancing care accessibility.
Person-Centered Care: A patient-centric approach is gaining traction globally, focusing on individualized treatment plans and shared decision-making. This trend aligns with Kaiser Permanente’s philosophy of empowering individuals to take an active role in their mental health journey.
The implementation of similar facilities varies across regions, influenced by local healthcare infrastructure, cultural norms, and funding mechanisms:
North America: The United States and Canada have seen a proliferation of integrated care models inspired by Kaiser Permanente. These facilities often collaborate with community-based organizations to provide comprehensive services.
Europe: In European countries, there is a growing focus on early intervention and prevention strategies. Some nations are establishing mental health hubs within primary care networks, similar to the Kaiser model.
Asia Pacific: The region’s diverse healthcare systems are adopting elements of integrated care, with some countries investing in community-based mental health centers. Japan, for instance, has implemented a model where mental health professionals work alongside general practitioners.
The economic landscape surrounding Kaiser Permanente mental health facilities is complex and multifaceted:
Funding Sources: These facilities typically rely on a combination of public and private funding. Government healthcare programs, insurance providers, and patient copays/deductibles contribute to their operational budget.
Market Demand: The demand for mental health services is influenced by various factors, including rising awareness, changing social norms, and the increasing prevalence of mental health disorders. This demand drives investment in specialized facilities.
Cost-Effectiveness: Research suggests that integrated care models like Kaiser’s can reduce overall healthcare costs by improving patient outcomes and preventing unnecessary hospitalizations. This cost-effectiveness is a compelling argument for policymakers and investors.
Investment in Kaiser Permanente-style mental health facilities follows several trends:
Public-Private Partnerships: Collaborations between government agencies and private healthcare providers are common, leveraging each other’s strengths to enhance service delivery and efficiency.
Community Engagement: Investors often prioritize facilities that foster community partnerships, ensuring services meet the unique needs of diverse populations.
Technology Integration: Investments in digital infrastructure and telemedicine solutions are increasing, recognizing their potential to expand access and improve patient outcomes.
Technological advancements play a pivotal role in shaping the future of Kaiser Permanente mental health facilities:
Electronic Health Records (EHRs): The adoption of EHR systems enables seamless sharing of patient information across different care settings, enhancing coordination and continuity of treatment.
Telehealth Platforms: Video conferencing tools allow for remote therapy sessions, breaking down geographical barriers to access. Mobile apps can facilitate real-time communication between patients, therapists, and support staff.
Artificial Intelligence (AI) and Machine Learning: AI-powered chatbots and virtual assistants provide immediate support and guidance to individuals seeking mental health resources. Machine learning algorithms can analyze patient data to predict outcomes and personalize treatment plans.
These technological innovations have a profound impact on service delivery:
Improved Access: Telehealth expands access to care, particularly in underserved rural areas. Digital platforms enable individuals to seek support from the comfort of their homes.
Personalized Treatment: AI-driven tools can adapt treatment plans based on individual patient needs, enhancing the effectiveness of interventions.
Efficiency and Cost Savings: Streamlined processes and automated tasks reduce administrative burdens, allowing healthcare professionals to focus more on direct patient care.
The development and operation of Kaiser Permanente mental health facilities are guided by a web of policies and regulations:
Mental Health Parity Act (MHPA): This US federal law ensures equal coverage for mental health services, prohibiting discrimination in insurance plans. It aligns with the Kaiser model’s comprehensive approach to care.
Substance Use Disorder and Mental Health Services Block Grant: Funded by the US government, this grant supports state and local programs addressing substance use and mental health disorders, influencing facility development and service offerings.
National Institute of Mental Health (NIMH) Guidelines: NIMH provides evidence-based guidelines for treatment and management of various mental health conditions, guiding clinical practices within these facilities.
Policymakers play a crucial role in shaping the landscape of Kaiser Permanente-inspired facilities:
Reimbursement Policies: Government reimbursement rates and insurance coverage policies directly impact the financial sustainability of these facilities. Favorable policies encourage investment in similar models.
Regulatory Oversight: Licensing and certification requirements ensure facilities meet specific standards of care. These regulations can drive innovation by promoting the adoption of best practices.
Funding Initiatives: Government grants and funding programs targeted at mental health initiatives influence the development and expansion of these facilities.
Despite its successes, the Kaiser Permanente model faces several challenges:
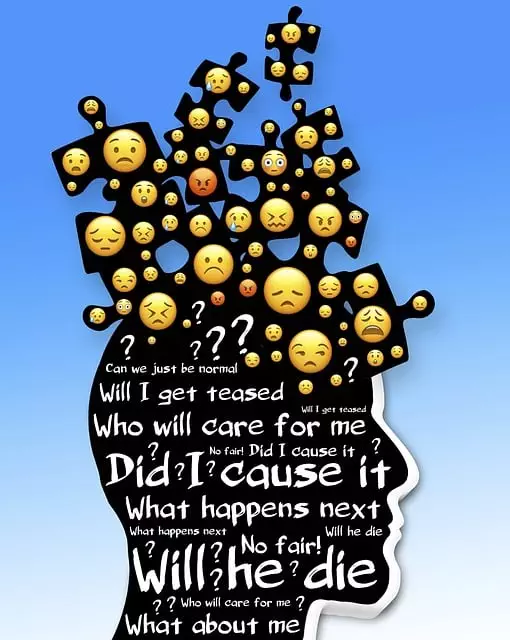
Stigma and Perception: Despite progress, stigma surrounding mental illness remains a barrier to access. Some individuals may perceive specialized mental health services as a sign of weakness or vulnerability.
Workforce Shortages: The demand for qualified mental health professionals often exceeds supply, particularly in rural areas. Attracting and retaining specialists is a persistent challenge.
Resource Allocation: Ensuring adequate funding and resources for these facilities is crucial but can be contentious, especially in times of budget constraints.
To address these issues, several strategies can be employed:
Public Awareness Campaigns: Proactive campaigns aimed at reducing stigma and promoting mental health literacy can encourage individuals to seek early intervention and support.
Education and Training Programs: Investing in training initiatives to expand the pool of mental health professionals, including school and community-based programs, can help address workforce shortages.
Public-Private Partnerships: Collaborating with businesses and community organizations can leverage additional resources and expertise, enhancing facility capabilities.
Several Kaiser Permanente mental health facilities have achieved notable successes, offering valuable lessons for the broader field:
Arvada’s Youth Mental Health Program: This program focuses on early intervention and prevention for youth aged 10-24. By integrating services within schools and community settings, it has demonstrated improved outcomes and reduced stigma among young people.
The Integrated Care Model in Seattle: Kaiser Permanente’s facility in Seattle implemented a comprehensive integrated care model, collaborating closely with primary care providers. This approach led to significant improvements in patient retention and clinical outcomes, serving as a model for other healthcare systems.
Telehealth Success in Rural Areas: A Kaiser Permanente initiative in rural Colorado utilized telehealth to provide specialized mental health services to underserved communities. The program’s success highlighted the potential of digital technologies in expanding access and improving care coordination.
Looking ahead, the future of Kaiser Permanente mental health facilities holds exciting possibilities:
Personalized Medicine: Advancements in genomics and neuroscience will enable more personalized treatment approaches, tailoring interventions to individual patient profiles.
Digital Health Ecosystems: The integration of various digital tools, from wearable devices to AI-driven platforms, will create comprehensive health management systems, enhancing patient engagement and outcomes.
Community-Based Initiatives: Expanding partnerships with community organizations and schools will strengthen the reach and impact of these facilities, fostering a more supportive environment for mental well-being.
To capitalize on emerging trends, facilities should:
Embrace Digital Transformation: Invest in digital infrastructure and explore innovative solutions like AI-driven care coordination to enhance service delivery.
Foster Community Engagement: Collaborate with local organizations to develop tailored mental health programs that address unique community needs.
Focus on Research and Innovation: Encourage research partnerships to explore new treatment modalities and evaluate program effectiveness, ensuring continuous improvement.
The Kaiser Permanente mental health facility in Arvada represents a significant milestone in the evolution of mental healthcare, offering comprehensive, patient-centered services within a dedicated, integrated system. Its global impact and successful applications underscore the power of this model in transforming lives and communities. As we navigate the future, the lessons learned from facilities like Arvada’s will guide the development of even more effective and accessible mental health care systems worldwide.
Q: How does Kaiser Permanente ensure equal access to mental health services?
A: Kaiser Permanente prioritizes equity through policies like the Mental Health Parity Act, ensuring insurance plans provide equal coverage for mental health and substance use disorder services. They also collaborate with community partners to reach diverse populations.
Q: What role does technology play in improving mental health care?
A: Technology, from EHRs to telehealth platforms and AI tools, enhances access, personalizes treatment, improves efficiency, and enables better patient engagement. These innovations are key to the future of mental healthcare.
Q: How can stigma be overcome in seeking mental health services?
A: Public awareness campaigns, education initiatives, and celebrity advocacy can help reduce stigma. Facilities should create supportive environments and offer non-judgmental care to encourage early intervention and ongoing support.
Q: What are the key considerations for investing in mental health facilities?
A: Investors should consider market demand, funding sources, and community partnerships. The success of these facilities relies on effective collaboration, innovative technologies, and evidence-based practices.
Q: How can mental health facilities address workforce shortages?
A: Expanding training programs, offering incentives for specialists, and promoting interprofessional education can help attract and retain a diverse mental health workforce. Collaboration with educational institutions is essential in this regard.
Mental health education programs at facilities like the Kaiser Permanente mental health facility in…….
Mental wellness self-assessment tools are crucial for modern mental healthcare at facilities like Ka…….

Kaiser Permanente mental health facility Arvada is committed to exceptional risk management through…….
The text advocates for adaptability in personal and professional spheres, emphasizing a future-orien…….